From the Director:
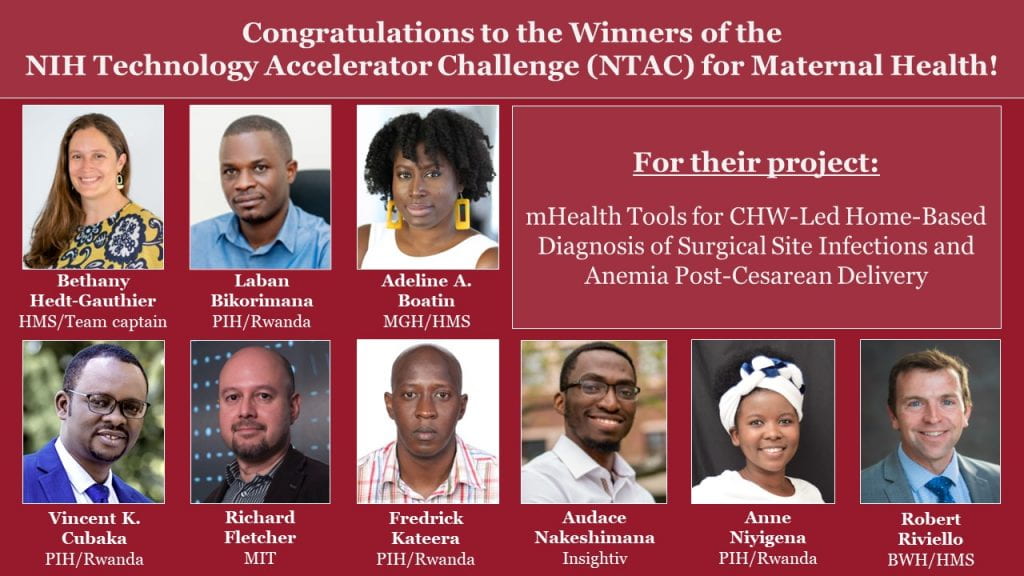
I am so excited to be able to inaugurate our Global Health Research Core’s website by announcing that Bethany Hedt-Gauthier and her team just won first place in the National Institute of Health’s Technology Accelerator Challenge for Maternal Health! The prize recognizes the group’s work in developing a mobile app that allows community health workers in Rwanda to diagnose surgical site infections and anemia during routine home visits to mothers who have delivered by Caesarian section. Read more about how it was developed and how it works below.
One of the reasons for the very high maternal mortality experienced in some low and middle-income countries is the lack of access to C-sections, especially among rural populations that can’t easily reach health facilities. And one of the reasons for high mortality after C-sections is the high rate of post-operative infection that can occur. Close monitoring of surgical sites requires either prolonged hospitalization or frequent return visits to health facilities for follow-up but this can place an insurmountable burden on a woman who has just had a C-section and who must walk long distances to reach a facility.
Bethany and her team created this tool to leverage the strong community health worker system in Rwanda that ensures that post-partum women can be followed up in their homes. But it is not enough to send a community health worker out to a home to ensure that a woman does not have an infection. As an infectious disease physician, I know that the diagnosis of a surgical site infection is not an easy one and certainly not one that community health workers can make in the context of a home visit without adequate lighting and medical instruments. Hence, the great value of the instrument that this team created, a tool that can be used by CHWs and that can identify women in need of further evaluation with excellent accuracy.
Our Core has existed now for more than a decade and our team (of mostly women) has been productive in terms of both academic output (research publications and grants) and of creative solutions to problems like this one. Among many other achievements, Molly Franke has developed an approach to community-based support for HIV-infected adolescents transitioning from pediatric to adult care in Peru and Ann Miller has championed interventions to ensure healthy early childhood development in many different contexts. I am hoping that in future, this new website will allow us to share our work in a more timely and accessible way. Please stay tuned.
Who are we?
We are a team of researchers, technologists, clinicians, and implementers that have worked together with the goal of providing higher quality and more accessible care to women delivering via cesarean in rural Rwanda.
Our NTAC prize team includes the individuals leading the most recent work:
Our extended team & supporters
Many people have contributed over the years, including: Monique Abimpaye, Barnabas Alayande, Joanna L Ashby, Paulin Banguti, Lisa M Bebell, Laban Bikorimana, Adeline A Boatin, Saddam Bukuru, Nissi Fidele Byiringiro, Teena Cherian, Leila Dusabe, Ziad El-Khatib, Ivan Emil, Eve Estrada, Kara Faktor, Paul Farmer, Richard Fletcher, Erick Gaju, Grace Galvin, Jean de Dieu Gatete, Andrea Goodman, Magdalena Gruendl, Regis Habimana, Caste Habiyakare, Sadoscar Hakizimana, Bethany L Hedt-Gauthier, Olivia Hughes, Holly Irasubiza, Ornella Kampayire, Prisca Kasonde, Fredrick Kateera, Daniella Kayitesi, Stefanie J Klug, Rachel Koch, Marthe Kubwimana, Frank Kwizera, Yihan Lin, Amy Luo, Martin Macharia, Hema Magge, Alexi Matousek, Christian Mazimpaka, Elizabeth Miranda, Rose L Molina, Abimpaye Monique, Tharcisse Mpunga, Joel Mubiligi, Betrand Mugabe, Megan Murray, Juliet Musabeyezu, Moses Muwanguzi, Evrard Nahimana, Deogratias Ndagijimana, Patient Ngamije, Joseph Ngonzi, Edison Nihiwacu, Anne Niyigena, Joseph Niyitegeka, Fulgence Nkikabahizi, Jonathan Nkurunziza, Theoneste Nkurunziza, Georges Nshimirimana, Marcel Nshunguyabahizi, Georges Ntakiyiruta, Naome Nyirahabimana, Alexandre Nyirimodoka, Jackline Odhiambo, Faith Odwaro, Olasubomi Olubeko, Jack M Omondi, Brittany L Powell, Siona Prasad, Bahati Ramadhan, Robert Riviello, Katharine Ann Robb, Niclas Rudolfson, John Ruhumuriza, Gilbert Rukundo, Stephen Rulisa, Christian Rusangwa, Félix Sayinzoga, Gabriel Schneider, Katherine Semrau, Mark Shrime, Allison Silverstein, Kristin Sonderman, Harsh Sonthalia, Gabriel Toma, Christine Minani Ufashingabire, Grace Umutesi, Illuminee Uwicyeza, Eline Uwitonze, Lotta Velin, Wendy Williams, Bonnie Wong, Lilian Wong, Marthe Yankurije.
This work is also possible through the funding and support received from numerous sources: Burke Fellowship (Harvard Global Health Institute); Dean’s Innovation Grant (Harvard Medical School); Global Health Research Core Funds (Harvard Medical School); Harvard-Dubai Center for Global Health (Harvard Medical School); Inshuti Mu Buzima; Milton Fund (Harvard University); National Institutes of Health; Partners In Health; Program in Global Surgery and Social Change (Harvard Medical School).
What specific problem are we solving and why is it important?
Cesarean sections (c-sections) are the most commonly performed procedure in women globally. Women who deliver via c-section are at risk for postpartum complications, including surgical site infections (SSIs) and anemia. Timely SSI and anemia treatment can reduce the risk of maternal morbidity and mortality.
Our team’s research on c-sections in rural Rwanda over the last eight years has pointed us to this current work.
- Nearly 11% of women who delivered via cesarean developed a surgical site infection.
- Women report that seeking cesarean follow-up care at health centers is physically and financially challenging.
- Cesareans are financially catastrophic for 1 in 4 women; this increases to 3 in 4 women when factoring in the costs of follow-up care.
Community health worker- (CHW-) led home-based follow-up could monitor women and provide timely care for post-cesarean complications, without the physical and financial challenges associated with facility based follow-up.

What is the integrated mHealth tool for CHW-led cesarean follow-up?
Our team is developing an integrated mHealth-tool to guide CHWs during home visits. The mHealth tool is being developed by Insightiv, a Rwanda-based tech start-up, based on core algorithms and computer vision software developed at MIT. The tool is built for an Android OS and will be “stand-alone”, meaning no features will require connection to internet or cell networks which is an important feature in some rural areas in Rwanda.
The tool will have three core functionalities:
1. CHW assessment of danger signs and advising on postpartum recovery.
The integrated mHealth tool includes a comprehensive assessment of the woman’s recovery and counseling prompts to ensure she feels confident in how she should care for herself post-cesarean.
This content was developed through a Delphi process that engaged clinical, program, policy, and research experts. Graphic designer Betrand Mugabe has developed images and icons to accompany text prompts for this content.
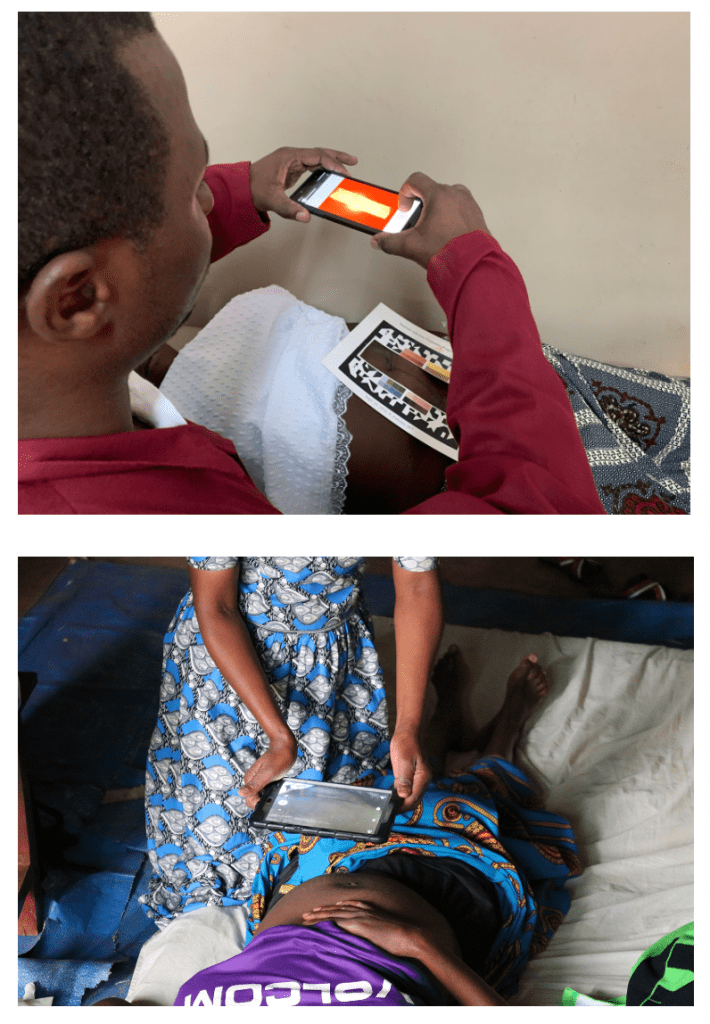
2. Surgical site infection diagnosis, using an image-based diagnostic algorithm.
With the mHealth tool, the community health worker can take an image of the wound and, with integrated mobile libraries, the image is processed and returns “infected” or “uninfected” diagnosis.
Over the last several years, our team has worked towards the surgical site infection prediction algorithms that are featured in the mHealth tool. The initial approach, which used a basic wound photograph, has a sensitivity=81% and specificity=65%.
Our team’s WoundScreener App standardizes image capture, provides real-time image preprocessing, and supports color calibration. As a result, newer algorithms trained on images collected with the WoundScreener App have higher specificity (specificity=75%) while maintaining the same sensitivity. Current work includes capacity to implement the color calibration and machine learning on the phone itself, and also adding real-time image quality feedback for the CHW at the time of capture.
Recently, our team has explored the use of thermal images for surgical site infection prediction algorithms. While this requires an additional device – costing about $200 per thermal camera – these algorithms are more accurate (sensitivity=95%, specificity=84%) and may be more generalizable to other populations.
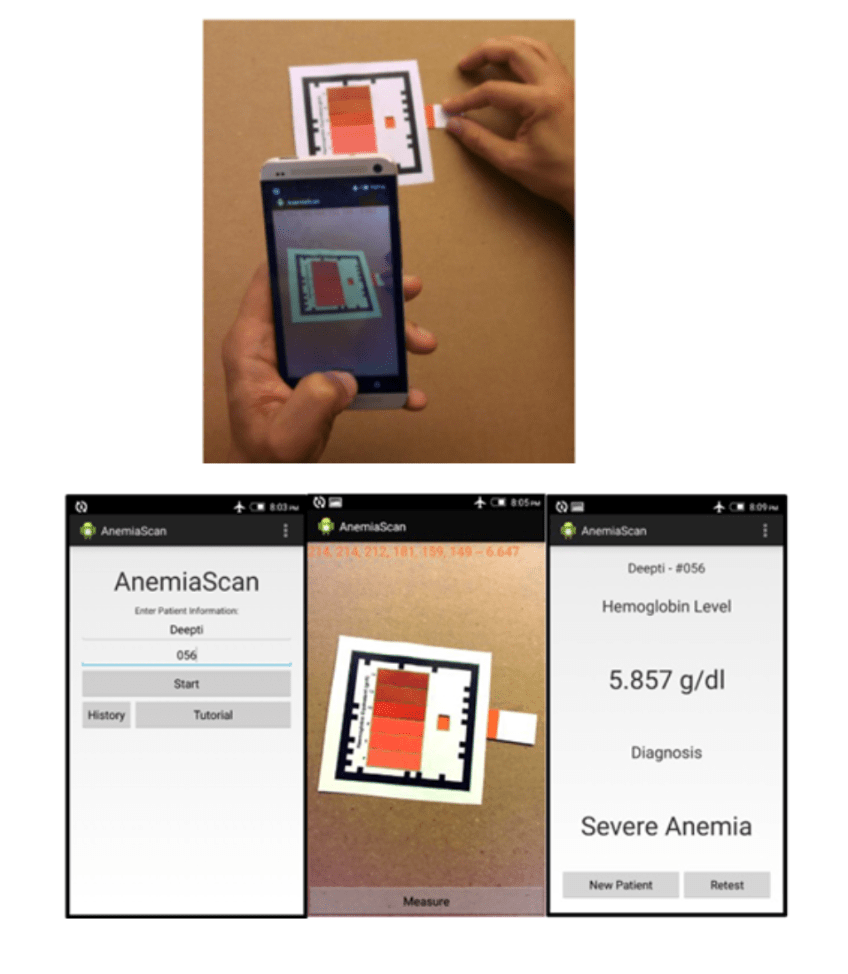
3. Anemia diagnosis, using computer vision to read colorimetric tests.
In our newest exploration, our team is working towards adding anemia diagnosis to the mHealth tool.
In earlier work, team member Rich Fletcher used computer vision to automatically generate results from standard anemia tests, removing human error from the manual color comparisons.
Over the next year, our team aims to validate these results in Rwanda, explore the potential of non-invasive anemia tests – i.e. tests that do not require a finger prick, such as under-eyelid or nailbed imaging – and to build these diagnostic tools onto the integrated platform.
Next steps and future work
We are currently building the integrated mHealth tool with input from community health workers, Ministry of Health officials, and research team members. With support from the National Institutes of Health, we will embark on usability and acceptability studies in Fall 2022 and prospective validation and evaluation studies in Fall 2023.
Future work includes:
- Furthering the surgical site infection diagnostic algorithm work:
- Validating the algorithms in diverse populations.
- Evaluating algorithms’ ability to predict infections earlier than day-of clinician review.
- Evaluating algorithms’ ability to detect the pathogen gram type for surgical site infections.
- Validating and building algorithms for anemia diagnosis.
- Integrating mHealth tools across multiple maternal and neonatal platforms.
Contact Information
For more information please contact Bethany Hedt-Gauthier at Bethany_Gauthier@hms.harvard.edu.









